Premature ventricular contractions (PVCs) are premature heartbeats originating from the ventricles of the heart. Premature ventricular contractions are premature because they occur before the regular heartbeat.
Normal function of the heart
The heart has four chambers. The upper two chambers are the atria, and the lower two chambers are the ventricles.
- The atria deliver blood to the ventricles, and the ventricles deliver blood to the lungs and to the rest of the body.
- The right ventricle delivers blood to the lungs while the left ventricle delivers blood to the rest of the body.
- The heartbeat (pulse) that we feel is caused by the contraction of the ventricles.
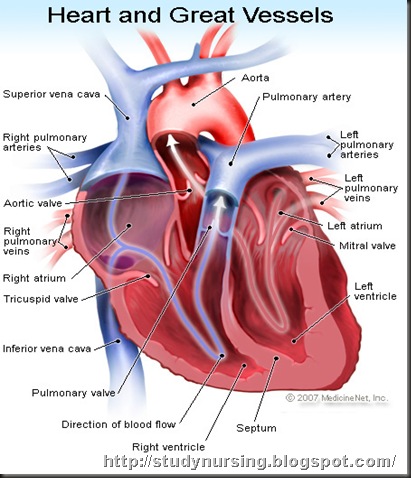 The heartbeat is normally controlled by the electrical system of the heart. The electrical system of the heart consists of the SA node (sino-atrial node), the AV node (atrio-ventricular node) and special tissues in the ventricles that conduct electricity.
The heartbeat is normally controlled by the electrical system of the heart. The electrical system of the heart consists of the SA node (sino-atrial node), the AV node (atrio-ventricular node) and special tissues in the ventricles that conduct electricity.
The SA node is the heart's electrical pacemaker. It is a small patch of cells located in the wall of the right atrium; the frequency with which the SA node discharges electricity determines the rate at which the heart normally beats. The SA node keeps the heart beating in a regular manner. At rest, the frequency of the electrical discharges originating from the SA node is low, and the heart beats at the lower range of normal (60-80 beats/minute). During exercise or excitement, the frequency of discharges from the SA node increases, increasing the rate at which the heart beats. In people who exercise regularly, the resting heart rate may be below 50-60 and is not of concern.
The electrical discharges pass from the SA node, through the special tissues of the atria into the AV node, and through the AV node to the special conduction tissues of the ventricles and causing the ventricles to contract.
What happens during a premature ventricular contraction?
During a premature ventricular contraction, the ventricle electrically discharges (and contracts) prematurely before the normal electrical discharges arrive from the SA node. These premature discharges are due to electrical "irritability" of the heart muscle of the ventricles and can be caused by heart attacks, electrolyte imbalances, lack of oxygen, or medications. Immediately after a premature ventricular contraction, the electrical system of the heart resets. This resetting causes a brief pause in heartbeat, and some patients report feeling the heart briefly stopping after a premature ventricular contraction.
How common are premature ventricular contractions?
Premature ventricular contractions are common. Many people have premature ventricular contractions without any symptoms. Premature ventricular contractions may be more common among older patients, patients with high blood pressure, and patients with heart disease. Premature ventricular contractions can also occur in young healthy individuals without heart disease or high blood pres
Causes
There are many causes of premature ventricular contractions, which include:
- heart attack;
- high blood pressure;
- cardiomyopathy, including congestive heart failure;
- disease of heart valves such as mitral valve prolapse;
- hypokalemia (low blood levels of potassium), and hypomagnesemia (low blood levels of magnesium), hypokalemia and hypomagnesemia can occur, for example, in patients taking diuretics (water pills);
- hypoxia (low amounts of oxygen in the blood), for example, hypoxia occurs with lung diseases such as emphysema or chronic obstructive pulmonary disease (COPD);
- medications such as digoxin (Lanoxin), aminophylline (Phyllocontin, Truphylline), tricyclic antidepressants, and ephedrine containing, decongestants;
- excessive intake of alcohol;
- excess caffeine intake;
- stimulant drug use such as cocaine, and amphetamines;
- myocarditis (heart muscle inflammation) and cardiac contusion (heart muscle injury), and
- premature 1ventricular contractions also occur in healthy individuals without heart diseases.
Symptoms
Patients with mild infrequent premature ventricular contractions often report no symptoms (asymptomatic) and are unaware of their premature ventricular contractions. Their premature ventricular contractions may be discovered when an electrocardiogram (ECG, EKG) is performed for a routine physical, insurance physical, or preoperative evaluation.
Patients with premature ventricular contractions sometimes report palpitations in the chest and in the neck. Palpitations are discomforting feelings due to forceful heartbeats. The heart beat immediately after a premature ventricular contraction is usually stronger (the heart ventricle contracts more forcefully) than normal. Patients with premature ventricular contractions may report feeling that the heart has stopped briefly. This is because there is usually a brief pause in heartbeat after a premature ventricular contraction when the electrical system of the heart resets. Moreover, the actual premature ventricular contraction beat may not be felt because the heart hasn't had time to fill with blood before beating so patients with PVC's often complain of "skipped" or "missed" beats.
Patients with frequent premature ventricular contractions such as bigeminy (every other heartbeat is a premature ventricular contraction), couplets (two consecutive premature ventricular contractions), or triplets (three consecutive premature ventricular contractions) often report no symptoms. But in rare occasions they may report weakness, dizziness, or fainting. This is because frequent premature ventricular contractions can diminish the ability of the heart to pump blood to the other organs (diminished cardiac output), resulting in low blood pressure.
Patients with three or more consecutive premature ventricular contractions in a row have ventricular tachycardia. Ventricular tachycardia that is prolonged can result in low cardiac output, low blood pressure, and fainting (syncope). Ventricular tachycardia can also develop into ventricular fibrillation, which is a fatal heart rhythm (see below).
What are the dangers of premature ventricular contractions?
Premature ventricular contractions in healthy individuals without high blood pressure and heart diseases do not pose any health risks. Premature ventricular contractions in patients with heart diseases (heart attacks, heart failure, diseases of the heart valves) may be associated with increased risks of developing ventricular tachycardia. Ventricular tachycardia is a sustained run of rapid ventricular contractions. Ventricular tachycardia is life-threatening because: 1) it occurs suddenly with no prior warning, and 2) it frequently develops into ventricular fibrillation. Ventricular fibrillation is a chaotic rhythm where the ventricles quiver rapidly in a purposeless fashion. The heart with ventricular fibrillation cannot pump blood effectively to the brain and the rest of the body. If untreated, ventricular fibrillation can be fatal within minutes. An estimated 250,000 Americans die in this way each year.
Many doctors believe that premature ventricular contractions do not necessarily cause ventricular tachycardias or ventricular fibrillations. Instead, premature ventricular contractions may be merely indicators (symptoms) of serious heart diseases or other serious conditions such as hypokalemia, hypoxia, and on-going heart damage from heart attacks, or medications such as digoxin and aminophylline toxicity. It must be emphasized that many premature ventricular contractions are harmless (benign) and not associated with structural heart disease. If the work up for underlying heart disease is unrevealing, the patient can be assured that their prognosis is excellent.
Diagnosed
There are two aspects in the diagnosis of premature ventricular contractions; detecting them, and diagnosing the underlying causes. Electrocardiograms (ECG EKG) and Holter monitors are used to diagnose premature ventricular contractions. EKGs, blood tests, echocardiograms, and cardiac stress tests are used to determine the underling causes of premature ventricular contractions.
Electrocardiogram (EKG, ECG)
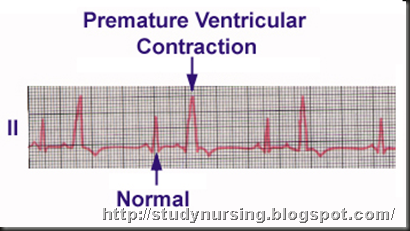 An electrocardiogram (EKG, ECG) is a brief recording of the heart's electrical discharges. EKGs can be performed in the doctors' offices, clinics, and hospital emergency rooms. Doctors frequently ask for a rhythm strip (a prolonged EKG recording) to be performed at the same time as EKG to increase the chances of detecting premature ventricular contractions and other abnormal rhythms. The premature ventricular contractions are easy to recognize on EKG and rhythms strips, provided premature ventricular contractions occur during the recording. EKG may also demonstrate other problems such as heart attacks, hypokalemia, digoxin toxicity, heart muscle thickening (hypertrophy) due to long term high blood pressure.
An electrocardiogram (EKG, ECG) is a brief recording of the heart's electrical discharges. EKGs can be performed in the doctors' offices, clinics, and hospital emergency rooms. Doctors frequently ask for a rhythm strip (a prolonged EKG recording) to be performed at the same time as EKG to increase the chances of detecting premature ventricular contractions and other abnormal rhythms. The premature ventricular contractions are easy to recognize on EKG and rhythms strips, provided premature ventricular contractions occur during the recording. EKG may also demonstrate other problems such as heart attacks, hypokalemia, digoxin toxicity, heart muscle thickening (hypertrophy) due to long term high blood pressure.
Holter monitor
A standard EKG and a rhythm strip performed at the time of a visit to the doctor's office may not detect the premature ventricular contractions because they may not be occurring at that moment. Holter monitoring is then necessary to detect the premature ventricular contractions in these patients with heart palpitations. A Holter monitor is a continuous recording of the heart's rhythm for 24 hours. Holter monitoring can be used diagnose premature ventricular contractions as well as other heart rhythm abnormalities such as atrial fibrillation, atrial flutter, and ventricular tachycardias.
Since more than 50% of middle aged men can have premature ventricular contractions during Holter monitoring, not all premature ventricular contractions found during Holter monitoring are clinically important. Doctors interpreting the Holter monitoring studies must take into account the patient's medical history in determining the importance of Holter monitor findings.
In patients with infrequent symptoms an event marker may be used in lieu of a Holter monitor as this can be worn for up to 30 days.
Echocardiography
Echocardiography uses ultrasound waves to produce images of the heart's chambers and valves and the lining around the heart (pericardium). Echocardiography is useful in measuring the size of the heart chambers, the forcefulness of heart ventricle contractions, the thickness of the heart muscles, and the functioning of the heart valves. Echocardiography is therefore useful in diagnosing conditions that can cause premature ventricular contractions such as:
- Mitral valve prolapse: Echocardiography can detect and measure the severity of mitral valve prolapse and other valvular diseases.
- Muscle hypertrophy: Echocardiography can detect heart muscle hypertrophy (thickening of heart muscle) as a result of long term high blood pressure.
- Heart muscle damage: Echocardiography can measure the extent of heart muscle damage from heart attacks or cardiomyopathy.
- Ejection fraction: Echocardiography can be used to calculate the ejection fraction of the left ventricle. Ejection fraction is a measure (estimate) of the amount of blood pumped during each contraction of the ventricle. Heart ventricles extensively weakened by heart attacks or cardiomyopathy will have low ejection fractions. Patients with low ejection fractions have higher risks of developing life threatening ventricular tachycardias and fibrillations than patients with normal ejection fractions.
Exercise cardiac stress test (treadmill stress test)
Exercise cardiac stress testing (ECST) is the most widely used cardiac stress test. The patient exercises on a treadmill according to a standardized protocol with progressive increases in the speed and elevation of the treadmill (typically changing at three minute intervals). During the ECST, the patient's electrocardiogram (EKG), heart rate, heart rhythm, and blood pressure are continuously monitored. If a coronary arterial blockage results in decreased blood flow to a part of the heart during exercise, certain changes may be observed in the EKG, including increase in premature ventricular contractions and development of ventricular tachycardias.
Adjuncts to ECST (stress echo and nuclear imaging)
Another supplement to the routine ECST is stress echocardiography. During stress echocardiography, the sound waves of ultrasound are used to produce images of the heart at rest and at the peak of exercise. In a heart with normal blood supply, all segments of the left ventricle (the major pumping chamber of the heart) exhibit enhanced contractions of the heart muscle during peak exercise. Conversely, in the setting of cardiovascular disease, if a segment of the left ventricle does not receive optimal blood flow during exercise, that segment will demonstrate reduced contractions of heart muscle relative to the rest of the heart on the exercise echocardiogram. Stress echocardiography is very useful in enhancing the interpretation of the ECST, and can be used to exclude the presence of significant cardiovascular disease in patients suspected of having a "false-positive" ECST. Alternatively, nuclear imaging may be used as an adjunct to ECST and may be even more sensitive in noninvasively detecting underlying coronary artery disease.
Blood tests in diagnosing causes of premature ventricular contractions
Blood tests for diagnosing conditions that can cause premature ventricular contractions include:
- blood electrolyte levels can be performed to detect low potassium or magnesium levels (hypokalemia and hypomagnesemia);
- blood drug levels can be performed to detect digoxin and aminophylline drug toxicity or thyroid levels, for example, an overactive thyroid may result in premature ventricular contractions;
- blood oxygenation (oximetry) can be measured to detect hypoxia;
- blood tests can be performed to detect illicit drugs, such as amphetamine abuse; and
- blood levels of cardiac enzymes [creatine phosphokinase (CPK), troponins (regulatory proteins)] can be performed to assess for heart muscle damage as a result of heart attacks.
Treatments
The reasons for treating premature ventricular contractions are:
1. to relieve symptoms of palpitation;
2. to treat conditions that cause premature ventricular contractions since many conditions that cause premature ventricular contractions are potentially life threatening; and
3. to prevent ventricular tachycardia and sudden death.
In healthy individuals without heart disease, premature ventricular contractions need no treatment. For relief of palpitations, one may consider the following measures:
- stop alcohol and caffeine intake;
- stop over-the-counter nasal decongestants that may contain adrenaline such as medications containing pseudoephedrine (certain weight loss supplements may aggravate premature ventricular contractions, and should never be used without consulting with one's physician);
- stop drug abuse such as amphetamines, cocaine; and
- stop cigarette smoking.
Conditions that can cause premature ventricular contractions can also be potentiality life-threatening. These conditions are often treated in hospital-monitored beds. Monitored beds are beds (or rooms) that are equipped to record the patients' heart rhythm continuously. Patients are also given intravenous medications. These conditions are:
- low potassium or magnesium levels (hypokalemia and hypomagnesemia) - potassium and magnesium can be given intravenously;
- digoxin and aminophylline toxicity: medications can be given to counteract drug toxicity;
- acute heart attack: medications and procedures (coronary angiogram and PTCA) are performed urgently to open blocked coronary arteries to restore blood supply to the heart muscle; and
- low blood oxygen levels (hypoxia): oxygen can be given nasally, and medications can be given to treat the underlying lung diseases.
Anti-arrhythmia medications
Anti-arrhythmia medications are used to control premature ventricular contractions with the goal of preventing ventricular tachycardias, ventricular fibrillations, and sudden death. Examples of anti-arrhythmia medications include beta-blockers, procainamide (Pronestyl, Procan-SR, Procanbid), amiodarone (Cordarone), and several others. Unfortunately, there is little scientific evidence that suppressing premature ventricular contractions with anti-arrhythmic medications prevent ventricular tachycardias, ventricular fibrillations, and sudden death.
Some anti-arrhythmia medications actually can cause abnormal heart rhythms. Thus anti-arrhythmic medications are only prescribed cautiously in patients at high risk of developing ventricular tachycardia and ventricular fibrillation; and usually initially in the hospital setting. This does not apply to beta-blockers, which are prescribed to many heart patients for many reasons, and not only do not accelerate arrhythmias, but usually decrease premature ventricular contractions. In many patients with premature ventricular contractions and significant underlying cardiac disease, or with severe symptoms, electrophysiology testing (EP) may be recommended. This is a test performed with catheters to see if a patient is at risk of life-threatening ventricular arrhythmias, which are treated with either medications or sometimes tiny implantable defibrillators.
![clip_image002[4] clip_image002[4]](http://lh6.ggpht.com/_byy_1rr1vTI/S_Y3_1TACXI/AAAAAAAAAmA/uD0yLdj168M/clip_image0024_thumb4.gif?imgmax=800)
No comments:
Post a Comment