Mechanisms of injury
- blunt injuries
- crush injuries
- penetrating injuries
- inhalation burns
- aspiration of foreign bodies
2 major forces within chest which lead to injury: compression and distraction. Compression results in destruction of vascular components, haemorrhage, oedema and impairment of function. Distraction injuries usually result in shearing forces which destroy integrity of intrathoracic viscera
Blunt trauma
- mode of injury important
- where there has been massive deformity of a car or a history of a fall of 5 metres or more major intrathoracic injuries should always be suspected. The physical nature of chest wall allows for considerable elastic recoil, especially in young patients and therefore degree of injury within chest may need to be judged initially by deformity to car rather than appearance of patient
- blunt injuries occur in 3 major directions: AP, lateral and transdiaphragmatic
- AP deformity results in relative backward motion of heart. This may result in disruption of aorta at level of ligamentum arteriosum just below left subclavian. As heart swings back and up it may cause so-called wishbone # of a proximal bronchus
- injuries to heart occur in up to 1/2 of patients after deceleration injuries
- deceleration with impact to back causes relatively few intrathoracic injuries
- lateral compression of chest during deceleration causes fractures typically of lower ribs with risk of injury to liver, spleen and kidneys
- when lateral compression results in flail segments damage to thoracic cavity is usually relatively small and most frequently limited to contusion and laceration of lung parenchyma
- lap belt of seat belts leads to rise in intrabdominal pressure in massive deceleration and this, combined with shearing and twisting of upper trunk may result in diaphragmatic rupture
Penetrating injuries
- result in parenchymal damage related to track of missile or stabbing implement and velocity
- more solid structures (eg heart and major vessels) suffer greater injury where high-velocity missiles are penetrating weapon
- most lethal complication is haemorrhage
- often associated with abdominal trauma
Crush injury
- occurs where elastic limits of chest and its contents have been exceeded
- patients usually have AP deformity
- majority have flail chests with multiple fractures, pneumothorax or haemothorax
- most have pulmonary contusion
- injuries of heart, aorta, diaphragm, liver , kidney and spleen are common
- another group of patients with crush injuries are those with "traumatic asphyxia" syndrome, where constrictive forces are applied over a wide area for as little as 2-5 mins. Profound venous hypertension associated with relative stasis is mechanism of injury. There is widespread capillary dilatation and rupture, subconjunctival haemorrhage and retinal haemorrhage. Simultaneous injuries (eg intracranial haemorrhage) must be suspected
- severe crush injuries have a high mortality
Chest trauma haemodynamics
- hypovolaemia most important mechanism
- cardiac tamponade
- myocardial contusion
- valve injury
- intracardiac shunt
Chest trauma hypoxia
Due to:
- reduced blood volume
- ventilatory failure
- contusion
- displacement of mediastinum
- pneumothorax
Clinical features:
Initial history and examination are often abbreviated
Examination
- air hunger; use of accessory muscles; tracheal deviation; cyanosis or distended neck veins; (evidence of tension pneumothorax, or tamponade);
- tracheal deviation (evidence of tension pneumothorax)
- major defects in the chest (sucking chest wounds);
- unilaterally diminished breath sounds or hyperresonance to percussion (evidence of closed pneumothorax or tension pneumothorax);
- decreased heart sounds (pericardial tamponade);
- location of foreign bodies;
- location of entry and exit wounds.
Investigations
CXR
- CXR most useful screening investigation
- Look for subcutaneous air, foreign bodies, bony fractures, widening of mediastinum, pneumothorax, pneumomediastinum, pleural fluid, pulmonary parenchymal abnormalities(infiltrates, atelectasis etc)
- Check ETT, and other hardware.
- Inspiratory/expiratory films for checking for pneumothorax.
- supine AP film Þ some conditions have different radiological features. Look in particular for the following:
- pneumothorax: (NB up to 30% of pneumothoraces missed on supine CXR) air collects in anterior-inferior pleural space producing:
- "deep" costophrenic sulcus (image)
- "double-diaphragm" contour +/- depression of hemidiaphragm
- hyperlucency in lower thorax and upper abdomen
- sharp demarcation of cardiac apex
- visceral pleura at base of lung may be outlined
- pneumomediastinum:
- parietal pleura visible along left mediastinal border. NB pleura descends below mid-hemidiaphragm
- sharply defined edge to descending aorta which can often be followed into upper abdomen
- "continuous diaphragm" sign under cardiac shadow
- subcutaneous, retroperitoneal or intraperitoneal emphysema
- pneumopericardium
- air around heart that does not rise above level of pericardial reflection at root of great vessels
- air shifts with position of patient (unlike pneumomediastinum)
- pleural effusion:
- uniform increase in density over hemithorax
- pleural cap
- pulmonary contusion:
- homogenous infiltrates that tend to be peripheral and non-segmental
- may be associated with adjacent rib fractures
- air bronchograms are rare due to blood in small airways
- ruptured hemidiaphragm:- more commonly left sided
- non-specific signs include: apparent elevation of hemidiaphragm, obliteration or distortion of contour of hemidiaphragm, contralateral displacement of mediastinum, pleural effusion
- presence of gas containing viscera in thorax, particularly with a focal constriction across gas-containing bowel is pathognomonic
- haemopneumothorax may be misdiagnosed when dilated stomach gives horizontal air-fluid interface on erect CXR
- in absence of right rib #s a small right haemothorax with a "high R diaphragm" suggestive of ruptured diaphragm
- findings may be absent in 25-50% initially
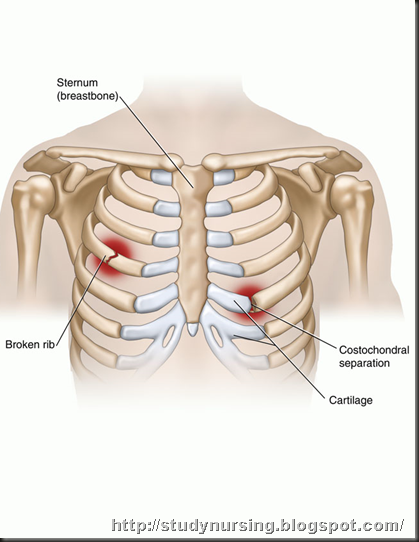
- chest wall injuries:
- may give clues to associated injuries
- fractures of first 3 ribs in particular indicates significant trauma
- thoracic outlet fractures associated with brachial plexus or vascular injuries
- subclavian vascular injury should be suspected in patients with fractures of first 3 ribs, clavicle and scapula, particularly when associated with significant fracture displacement, extrapleural haematoma, brachial plexus neuropathy or radiological evidence of mediastinal haemorrhage (image)
- fractures of sternum are rare and require both lateral and oblique views of thorax for diagnosis. The presence of a fractured sternum and an abnormal mediastinal contour should prompt a search for injury to great vessels
- haemopericardium:
- NB rapid accumulation of blood in pericardial space often causes cardiac tamponade wthout altering appearance of cardiac silhouette
CT Scan
- Valuable tool
- Aids in diagnosis and precise location of numerous lesions.
- Contrast is useful particularly when looking for mediastinal haemorrhage and periaortic haematomas.
Echocardiography
Cardiac wall motion abnormalities and valve function and presence of pericardial fluid or blood.
ECG
Most common abnormality in thoracic trauma are S-T and T wave changes and findings indicative of bundle branch block
Angiography
Remains the gold standard for defining thoracic vascular injuries
Bronchoscopy
Indications include evaluation of airway injury, haemoptysis, segmental or lobar collapse, and removal of aspirated foreign bodies.
Management
Immediate management
- assure patent airway, oxygenation and ventilation
- exclude or treat:
- pneumothorax
- haemothorax
- cardiac tamponade
- assess for extrathoracic injuries
- decompress stomach
- provide pain relief
- reconsider endotracheal intubation, ventilation. In particular take into account gross obesity, significant pre-existing lung disease, severe pulmonary contusion or aspiration, need for surgery for thoracic or extrathoracic injuries
General management
Treatment of specific injuries
Monitoring
Should include follow-up CXRs. Common for patients with pulmonary contusion to deteriorate in first 24-48 hrs following injury. Not necessarily due to progression of contusion but is more often due to development of pneumothorax, haemothorax, atelectasis or pulmonary oedema. For this reason serial CXRs are necessary in first 24 hrs
Following are danger signs requiring full reassessment:
- resp rate > 20/min
- heart rate > 100/min
- systolic BP < 100 mmHg
- reduced breath sounds on affected side
- Pao2 < 9 kPa on room air
- Paco2 > 8 kPa
- increased size of pneumothorax, haemothorax or increased width of mediastinum on CXR
Deterioration in any of these signs must be followed by a search for evidence of blood loss, tension pneumothorax, head injury, sepsis or fat embolism. Chest drains should be checked for patency
Chest drains
Indications for insertion of chest drains in stable patients:
- pneumothorax > 10% in non-ventilated patient (ie >1 intercostal space)
- haemothorax > 500 ml (ie above neck of 7th rib)
- surgical emphysema
- confluent opacity of lung field in a supine CXR suggesting haemothorax
There are arguments both for and against the insertion of prophylactic chest drains in patients with rib fractures who are to be ventilated for a GA. However without air or fluid draining the drain is likely to become blocked at an early stage. In a series of patients with blunt chest trauma one pneumothorax occurred per 79 days of ventilation when prophylactic drains were used as opposed to one per 62 days when they were not. Complication rate associated with insertion 6-9%
Theoretically, all that is required to drain pneumothorax is a small-bore tube but this is more likely to become blocked. When blood or pus is to be drained in an adult a 32 FG tube is recommended
Antibiotics
- use of prophylactic antibiotics controversial. Some recommend them for patients treated conservatively in whom a chest drain is inserted
- cefuroxime and metronidazole for patients with perforated viscus (in addition to exploration and drainage)
General measures:
- pain relief (eg pleural block)
- physio
- humidification
- bronchodilators (especially smokers or those exposed to smoke, irritant chemicals or those with tracheobronchial burns)
- consider cricothyroidotomy or "minitracheostomy" for those in whom general measures insufficient
Bronchoscopy
Indications for flexible bronchoscopy:
- massive air leak
- failure of lung to re-expand
- lobar collapse
- diagnosis and assessment of tracheal burns
- bronchial toilet
Rigid bronchoscopy has less of a role in the trauma patient but may be used in cases of persistent lobar collapse to aspirate a blood clot or plug of sputum
Mechanical ventilation
- most centres use PCV or PSV to reduce incidence of barotrauma
- PCV and PSV also provide some compensation for air leaks
Analgesia
Of extreme importance in determining whether deep breathing and coughing possible. Options:
- IV opioids in frequent small doses or by continuous infusion
- Entonox inhalation during physiotherapy
- intercostal nerve block:
- multiple individual nerve blocks (rptd as necessary)
- single large volume (eg 20 ml 0.5% bupivicaine) into 1 intercostal space. Spreads to block nerves above and below
- intrapleural bupivicaine via intercostal catheters using intermittent injections or continuous infusions
- epidural LA/opioids
- NSAIDs: fully resuscitated patients with normal renal function
Post-operative intensive care
- following tracheobronchial, lung or diaphragmatic repair high inflation pressures should be avoided
- tracheal suction must be minimal where there is a tracheobronchial suture line
- avoid fluid overload
- prevent gastric distension

No comments:
Post a Comment